The Denneroll Orthotic: I Didn’t Believe It Till I Tried It!
 Tuesday, July 13, 2010 at 7:24AM
Tuesday, July 13, 2010 at 7:24AM 
Joseph Ferrantelli, DC
Private Practice New Port Richey, FL
CTO CBP® Seminars
CEO PostureCo.
INTRODUCTION
Since the introduction of the Denneroll, many doctors have confronted us at seminars believing that there is simply no way a “simple orthotic” could get some of the spinal changes we have been obtaining. Well at first, I did not ‘believe’ Dr. Harrison either! Why should I without proof, after all that is the CBP moto, “Don’t accept something for truth that for which there is a lack of confirming evidence.” Well, Dr. Harrison already had tested this unit in Australia and I saw his preliminary findings – which were quite impressive, but until you start having cases for yourself, it was still hard to believe. While we are working on studies on this and other home methods of rehab to publish, I would like to share 4 cases with you out of my own office. Three of the following were performed with the Denneroll orthotic ONLY as the choice of spinal traction.
While I did not set out to perform any “Denneroll Only Traction protocols”, three of these patients could not perform in office traction as will be explained, with the forth electing for both office rehab methods as well as home Denneroll orthotic use.
Patient Case #1
In the first case, we have a female that was involved in a frontal collision crash. The subjective complaints were the typical complaints seen with whiplash injuries, such as neck pain, sclerontonegous referral to lower neck and upper thoracic spine from facet joint injury, headaches, etc. In this case, the patient elected simply not to perform in office traction due to time constraints. In office care consisted of initial coarse of acute care diversified adjusting for 6 visits, then CBP Mirror Image drop table and instrument based adjustments and Exercises.
The patient having such a magnitude of kyphosis, was started as soon as possible with the Denneroll orthotic (on her 7th visit) starting 2x/day at 1 minute and building up to two sessions of 10 minutes, once in morning, and again once at night. Once this goal was achieved, after 2 weeks (4 weeks after injury), she was placed on 1 session of use per day working up to 20 minutes daily. Her initial x-ray was performed on 10/6/2009 then the next post was actually only 2 weeks later, this time on a Digital Motion X-Ray, dated 10/20/2009. DMX was chosen as she persisted with headaches and I wished to better view any evidence of ligamentous laxity. Notice in just 2 weeks of use, the cervical kyphosis is reduced! After 40 sessions of home use, and 36 visits total treatments, with her symptoms and outcome studies showing her nearing MMI, she was prescribed another follow up Digital motion x-ray. The changes were quite amazing as evidenced below in Figure 1.

PostureRay® Analysis from 10/6/2009 to 3/24/2009
![clip_image002[5] clip_image002[5]](http://lh5.ggpht.com/_TwOomLHsIQE/TDf53bLweOI/AAAAAAAABt8/mJ9o2KNLp3o/clip_image002%5B5%5D%5B4%5D.jpg?imgmax=800)
Patient Case #2ab
On the next 2 cases, both patients, being friends which were involved in a low speed rear impact collision. Responding quite fast to acute care adjusting after10 visits, they were placed on Mirror Image protocols. However, at this initial re-exam, for both patients, their pain was down to 1/10 for complaints and neck disability scores, and SF36 scores, showing near resolution of any and all interference with activities of daily living, I had to promote them to a supportive care regiment. Remember, when treating injury cases, our job to return the patient to “pre-Injury” status, and both of these clients, knowing they had no other objective findings nor significant subjective complaints, I placed them on the supportive schedule of 1-2x/month with daily use of the Denneroll. I had to do some sort of home care, because I knew that their spines could not have been corrected with simple acute regiments of care.
Case 2a
In case 2a, the patient worked up to using the Denneroll for 20 minutes 1-2x/day, for a total of 40 total sessions along with Mirror Image Exercises. At the time of his final MMI examination and only a total in office treatments of 17 sessions, the outcome was quite amazing.
Figure 2a. |
 |
PostureRay® Analysis |
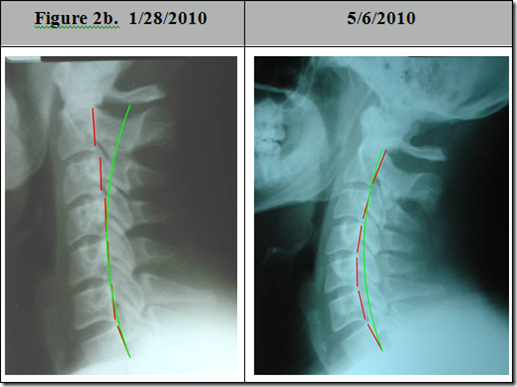
In case 2b, the occupant was in the vehicle as discussed with case 2a. The difference here is that the patient had significant laxity distally, and was instructed to use the Denneroll mid cervical spine, not lower cervical spine. Unfortunately, the patent, finding this much more difficult, placed the orthotic in his low neck - unbeknownst to the treating doctor, ie. myself! Again, his results were posted after 15 total in office visits. He had approximately 40 sessions of home use working up to on average 20 minutes per day on the Denneroll unit. All outcome scores continued to show nearly resolution of any and all complaints. However, due to the lack of compliance on the part of patient 2b, placing the orthotic too low, he actually “over corrected” his spine, leading to a significant hyperlordosis. I have never encountered such a finding with any home traction device, but it makes sense given his injuries and laxity distally in his spine, and the patient, weighing approximately 265 lbs, using the home orthotic with a large skull, creates quite significant force.
The point here is simple, the Denneroll orthotic is not to be taken lightly, it is not a toy, rather a home clinical device, and as such will change the spine if used, and as evidenced positioning is quite important. Patient compliance and training is a priority, and we recommend follow up quiz’s for placement so the patient can demonstrate the proper positioning. Even though the patient demonstrated proper use and placement of the unit on several occasions prior to obtaining a unit for home use, he placed it too low – due to comfort, which had deleterious effects. Even though the patient is still asymptomatic with no positive findings, I elected AGAIN to stress the importance of placement yet to the patient, moving the unit to mid to upper neck, but only using 2-3x per week for 10 minutes, along with home distraction traction 3 days a week for 20 minutes in order remove some of the lordosis distally. He is scheduled to have another follow up x-ray to check his progress again in approximately 2 months.
Figure 2b. |
|
 |
|
PostureRay® X-Ray Analysis![clip_image002[7] clip_image002[7]](http://lh4.ggpht.com/_TwOomLHsIQE/TDhmA9-kp_I/AAAAAAAABuU/f-NooHi2ATQ/clip_image002%5B7%5D%5B5%5D.jpg?imgmax=800) |
Given these cases, I (Dr. Joe F) now “believe” in the Denneroll orthotic as a viable addition to a patient’s home care, alongside other devices such as the Compression Extension Traction unit, and Circular Traction’s Cervical Remodeling Collar depending on their posture and cervical alignment - each, having specific applications to specific neck configurations.


For more information on the Denneroll Orthotic, please visit www.idealspine.com
 CBP Seminars | Comments Off |
CBP Seminars | Comments Off |