Colorful Olympic Tape for our Patients – TAPING MOVEMENT, NOT MUSCLES
 Tuesday, December 18, 2012 at 11:48AM
Tuesday, December 18, 2012 at 11:48AM 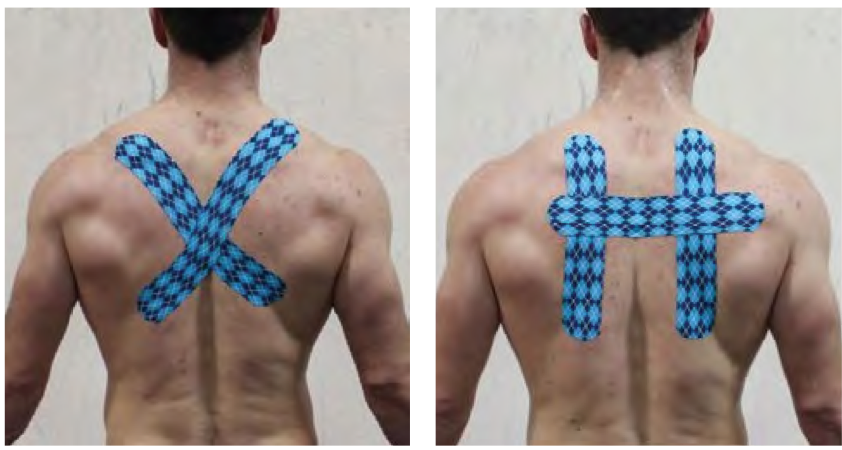
 Steven Capobianco D.C, DACRB, CCSP
Steven Capobianco D.C, DACRB, CCSP
Medical Director, Rock Tape.
www.rocktape.com
INTRODUCTION
“Kinesiology tape” was first used by acupuncturists and chiropractors in Japan over 20 years ago. Today it is used by practitioners throughout the world in the treatment of injuries and to improve sports performance.
It was apparent that world-class athletes were seeking an alternative to managing pain and maximizing recovery potential at the 2012 London Olympic Games. Practitioners and spectators alike witnessed athletes, from the diving platform to track and field, wearing colorful tape in intricate patterns and with questions of what it was, word began to spread.. While the use of kinesiology tape is often associated with athletes, the reality is that kinesiology tape is effective for a wide variety of problems, not just sports injuries.
The evidence supporting the role of kinesiology tape still lacks high-level clinical trials, but if you spend the time to research further you will start to see a trend. This trend was spearheaded by Thibaud (Feb 2011), and reported the effects of taping the skin in subjects that are compromised, either fatigued or injured. They found that the skin acted as an auxiliary kinesthetic system providing the brain with postural awareness when the compromised muscle/joint receptors were fatigued.

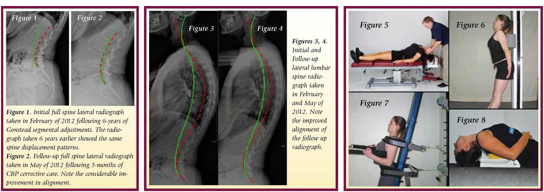
Kinesiology tape, developed and refined for the past 35 years, attempts to mimic the qualities of the skin in its elasticity and thickness. With these qualities in mind, the tape is applied on the skin in certain patterns to enhance certain physiological processes. Once applied to the skin the elastic capacity of the tape provides a light shear augmenting the mechanoreception of the area addressed. This same elastic recoil aids in pulling the epidermis and dermis layers of skin away from the underlying fascial compartments, thus improving fluid dynamics (acute/chronic edema) (Ya-Hui Chou). Both of the above processes have a substantial benefit in down-regulating nociception (pain), in return improving movement patterns in accordance to the area addressed with tape. Lastly the tape in its ability to enhance kinesthetic awareness through skin stimulation, can improve postural dysfunction. Careful application of tape along “fascial strain lines” has been shown to improve common postural dysfunctions such as upper and lower cross syndromes, hyper and hypolordosis, anterior/posterior tiling of the pelvis, and more (see figure 1).
SUMMARY
The refinement of kinesiology taping has extended from the traditional anatomical (muscle) applications to the more integrated fascial (movement based) applications. This innovative way of taping has revised some new and improved taping applications that have shown to improve movement dynamics, such as postural sway associated with compromised environment like pain and fatigue states, as discussed earlier in the science of taping. Athletes, such as those in the Olympic Games, are interested in the advancement of taping technology. With this added interest in “legal” performance enhancement which doesn’t involve drugs, athletes and coaches are looking for an edge in other alternatives including kinesiology tape. By enhancing our body awareness via movement taping, we can improve the length-tension relationships of the associated muscles, and, in turn, improve the neuromuscular efficiency of the intended activity.
Recently, the Garmin-Barracuda professional cycling team has implemented this model of taping to improve postural position on the bike to optimize power outputs during long cycling time trials. The team’s physicians believe that the tape, applied in specific patterns, improves form which translates to a faster time with less incidence of injury. This all translates into improved performance without the use of illegal enhancements. Future studies on the effects of stimulating the largest organ in our body (the skin) via kinesiology tape, is a new direction to investigate with regards to improving proprioception, posture and performance.
References
- Fuller, R.B. 1975. Synergetics. New York: Macmillan
- Ya-Hi Choi, et al. Manual Lymphatic Drainage and Kinesio Taping in the Secondary Malignant Breast Cancer-Related Lymphedema in an Arm With Arteriovenous Fistula for Hemodialysis. American J. of Hospice and Palliative Med. 00 (0) 1-4, (2012).
- Fascia Congress. 2009. www.fasciacongress.org/2009
- yers, T.W. 2009. Anatomy Trains: Myofascial Meridans for Manual and Movement Therapists. New York: Churchill-Livingston.
- Thibaud, et al.Degraded postural performance after muscle fatigue can be compensated by skin stimulation. Gait and Posture 33 (2011) 686-689.
- Hyun Mo An, et al. The effects of kinesio tape on lower extremity functional movement screen scores. International J. of Exercise Science 5 (3): 196-204 (2012).
 CBP Seminars | Comments Off |
CBP Seminars | Comments Off |  Chiropractic BioPhysics,
Chiropractic BioPhysics,  rocktape
rocktape