American Journal of Clinical Chiropractic
 Tuesday, July 17, 2012 at 11:49PM
Tuesday, July 17, 2012 at 11:49PM  CBP Seminars | Comments Off |
CBP Seminars | Comments Off |  Chiropractic BioPhysics
Chiropractic BioPhysics  Tuesday, July 17, 2012 at 11:49PM
Tuesday, July 17, 2012 at 11:49PM  Chiropractic BioPhysics
Chiropractic BioPhysics  Tuesday, July 17, 2012 at 11:16PM
Tuesday, July 17, 2012 at 11:16PM  Paul A. Oakley, M.Sc., DC
Paul A. Oakley, M.Sc., DC
CBP Research & Instructor
Private Practice New Market, Ontario, Canada
INTRODUCTION
Last issue we discussed the essential reasons for the understanding of contemporary ergonomics concepts and their potential contradictory effects on patient care – good ergonomic practices will aid in patient response to care - poor ergonomic practices will undeniably compromise patient outcomes. We have discussed the first two concepts, and now continue with concept 3 of 5.
3) Optimal Spinal Loading: Not too Much, Not too Little
A common ergonomic misconception is that recommendations should be directed at minimizing tissue loading, however, this is not true.1 For example, not typically considered stressful to the spine, sleeping for more than 8 hours at a time may indeed stress the spine.1 This is due to the fact that the discs swell by imbibing fluid over night,2 and since the discs function to transmit force, (rather than absorb force which is the function of the vertebral bodies)3 the column is subjected to increased stiffness and is at greater injury risk in the early morning.4 The fact is too much loading or too little loading is potentially injurious. For this reason, “the challenge is to develop a wise break strategy to facilitate optimal tissue adaptation.”1
Since most spinal injury occurs as an accumulation of micro-trauma as opposed to an isolated acute traumatic event,5,6 regular ‘micro-breaks’ are recommended. This allows a continuously varying demand and subsequent migration of load on the low back tissues.1 Standing up to answer the telephone while performing seated work is a good way to aid in varying the posture throughout the day. Any posture adopted for prolonged periods may fatigue the tissues used to maintain that position. When standing for long periods one can alternate the placement of a foot on top a footrest to reduce tension in the psoas and lumbar spine.7 See Figure 1.
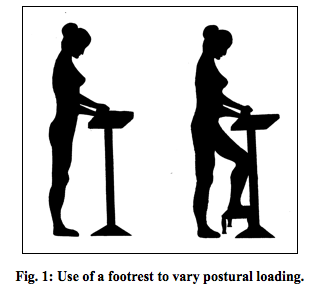
The idea of an ideal sitting posture is a farce. This is because it would only be ideal for about 10 minutes1 as sitting creeps the posterior ligamentous tissues (20 minutes of continuous sitting requires over 30 minutes of non-seated recovery time to regain the normal protective spine stiffness8). The ideal sitting posture is a variable one.9,10 McGill (2002)1 suggests three recommendations for prolonged sitting: 1) Use an ergonomic chair properly (i.e. vary the adjustable features regularly within sensible ranges); 2) Get out of the chair (i.e. rest breaks should involve opposite activities – Mirror Image Postures); 3) Perform an exercise routine during the workday (i.e. not first thing in the morning; not exercises that exert excessive spinal loads).
4. Reduce the Reaction Moment
The ‘reaction moment’ is the rotational force your body must generate to successfully perform a sagittal lift - the weight of the load (and upper limbs) would cause your torso to fall forward unless the back extensors offset this gravity-induced moment to allow the maintenance of an upright lift. The extensor activity within the low back causes compression of the spinal mechanism.11 Excessive compression within the low back is detrimental especially during prolonged, or repeated tasks. Excessive loading of the low back due to reaction moments can occur during any activity where there is a demand for the body to resist a force that is a distance from the spine.
Reducing the reaction moment is the key to reduce spinal compression. This is accomplished by carrying the load closer to the body and/or reducing the weight of the load lifted. See Figure 2.
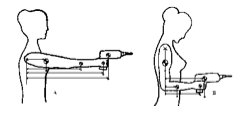
Fig. 2: Reduction of ‘reaction moment’ and therefore muscle work is accomplished by bending the arm to decrease distance of arm segments and load from spinal axis.
A third method of reducing a reaction moment is to direct the transmissible vector through the low back. The ‘transmissible vector’ is likened to the former concept only applied to tasks such as pushing and pulling. It should be known that there is no specific muscle that has the primary function of producing torso torque, it is performed by co-contraction of all the torso muscles resulting in substantial spinal loads.1 Thus, when performing tasks such as pushing and pulling on objects such as doors and vacuums, the pull/push should be directed so that it is in line with the low back.
5) Maintain Spine Stability
McGill was the first to capture a ‘live’ segmental spinal buckling while viewing the spine of a power lifter during a lift.12 This buckling is possible when either there were high forces in the global muscles and low forces in segmental muscles or when there are low forces in all muscles.13 This mechanism explains how one can injure themselves by performing ‘negligible’ lift such as picking up a pencil.5
As expressed by McGill, “stiffness creates stability,” and symmetrical stiffness offers greater stability.1 Thus, a slight abdominal co-contraction (5-10% max. vol. contraction) will ‘brace’ or stabilize the spine prior to a lift. This will prevent any tissue from bearing a surprise load.14 Spinal stability is also maintained by adopting symmetric postures, avoiding twisting action, and flexion postures. Symmetrical trunk postures also ensure greater available strength,15 enabling one to perform activities easier in symmetric postures.
Lastly, the lumbar lordosis is essential in maintaining spinal stiffness – keeping it dynamically (lifting) and having it statically (standing) – any chiropractic treatment neglecting the correction of lumbar lordosis is missing a key ingredient for their patient’s back stability and health.
Conclusion
It has been suggested that the “mechanics of the spine are not well understood by those who examine and treat these structures.”16 The Chiropractic BioPhysics® lumbar rehabilitation protocol has its unique niche in remolding the spinal posture and thus succeeding where most other LBP treatments fail including other chiropractic techniques. Both the neutral static posture and the dynamic postures performed throughout the day have significant implications for spinal health and response to treatment. The performance of a lumbar rehabilitation without regard for the dynamic activities performed throughout the day may render patient care fruitless. Always consider the Five Key Concepts to Lumbar Spine Ergonomics:
1. Maintain the Neutral Lumbar Curve
2. Appropriate Timing of Spinal Loads
3. Optimal Spinal Loading: Not too Much, Not too Little
4. Reduce the Reaction Moment
5. Maintain Spine Stability
References
1.McGill SM. Low back disorders: Evidence-based prevention and rehabilitation. Champaign, IL: Human Kinetics, 2002.
2.Urban JPG, McMullin JF. Swelling pressure of the lumbar intervertebral discs: Influence of age, spinal level, composition, and degeneration. Spine 1988;13:179-187.
3.Ruch WJ. Atlas of common subluxations of the human spine and pelvis. New York: CRC Press, 1997.
4.Adams MA, Dolan P, Hutton WC. Diurnal variations in the stresses on the lumbar spine. Spine 1987;12:130-137.
5.McGill S. The biomechanics of low back injury: implications on current practice in industry and the clinic. Journal of Biomechanics 1997;30:465-475.
6.Kumar S. Cumulative load as a risk factor for back pain. Spine 1990;15:1311-1316.
7.White III AA, Panjabi MM. Clinical biomechanics of the spine. 2 ed. New York: Lippincott Williams & Wilkins, 1990.
8.McGill SM, Brown S. Creep response of the lumbar spine to prolonged full flexion. Clinical Biomechanics 1992;7:43-46.
9.Eklund J. Biomechanical aspects of work seating. In: Kumar S, ed. Biomechanics in Ergonomics. Philadelphia: Taylor & Francis, 1999:325-334.
10. Pynt J, Higgs J, Mackey M. Seeking the optimal posture of the seated lumbar spine. Physiotherapy Theory & Practice 2001;17:5-21.
11. Troup JDG. Relation of lumbar spine disorders to heavy manual work and lifting. Lancet 1965;857-861.
12. Cholewicki J, McGill SM. Lumbar posterior ligament involvement during extremely heavy lifts estimated from flouroscopic measurements. Journal of Biomechanics 1992;25:17-28.
13. Cholewicki J, McGill SM. Mechanical stability of the in vivo lumbar spine: Implications for injury and chronic low back pain. Clinical Biomechanics 1996;11:1-15.
14. McGill SM, Norman RW. Low back biomechanics in industry: The prevention of injury through safer lifting. In: Grabiner MD, ed. Current Issues in Biomechanics. Champaign, IL: Human Kinetics Publishers, 1993:
15. Kumar S, Narayan Y, Zedka M. An electromyographic study of unresisted trunk rotation with normal velocity among healthy subjects. Spine 1996;21:1500-1512.
16. Paris SV. Anatomy as related to function and pain. Orthopedic Clinics of North America 1983;14:475-489.
 Chiropractic BioPhysics,
Chiropractic BioPhysics,  ergonomics
ergonomics  Tuesday, July 17, 2012 at 11:13PM
Tuesday, July 17, 2012 at 11:13PM 
Nona Djavid, DC
Private Practice Newport Beach, CA
MyChiroPractice, Inc.
CBP Certified Practitioner
Dr. Nona Djavid operates a private practice in Newport Beach, CA. A graduate of University of California at Berkeley in the field of Molecular and Cellular Biology with an emphasis in Neurology, Dr. Djavid earned her Doctorate of Chiropractic Degree from Life Chiropractic College West. She also earned post Doctorate certifications in Neurology and Chiropractic Biophysics. Dr. Djavid is the founder of WOW – Women of Wellness group – an organization that empowers female health care professionals to build healthy caring relationships through education and integrated health and wellness services.
INTRODUCTION
Years ago personal referrals and yellow page ads helped market and build businesses from the ground up. Small towns were littered with mom and pop shops, and business owners spent lazy afternoons walking up and down Main Street drumming up business with just a simple handshake and business cards.
Fast forward to today’s rapidly changing business landscape, and a new generation of technologically, web, and brand savvy patients who rely heavily on their FaceBook® friends for referrals, check the reputation of a health care provider on Yelp®, or Google® their way through dozens of listing for chiropractors, instantly trusting or discrediting them based on how each of their websites, logos, online reviews, or social media pages look like.
Right or wrong, image and social media standing is taking the front seat to credibility, reputation, or experience.
To stay competitive and visible, chiropractors have to start stepping outside the box, and give their future patients an image and presence that will make a statement. The first step would be to leave behind their homemade / cookie cutter logos and websites, and being open to change. Don’t get me wrong, I strongly believe one shouldn’t judge a book by its cover, but this new generation doesn’t even have time to crack open the book; an iPad® maybe.
How Do Quality Patients Choose a Chiropractor?
It’s very simple; aside from referrals, potential new patients let their subconscious decide. To understand this concept, you must put yourself in the shoes of a potential patient, and see the world through their eyes.
Let’s pretend you are looking to find a new dentist, because the referral from your wife happened to be on vacation. So you take to Google, and a minute later you are presented with a list of 20 dentists near your home.
As you click through to each dentist’s listings, you make certain conscious observations about them. You notice how fast or slow their website loads, how gimmicky or professional their web pages read, how attractive, old, or experienced the staff looks, or how depressing or modern their office feels. You may take a moment to read a couple of lines of text, but if the information is hard to find or decipher, you quickly click the back button.
For most people today, visual elements take precedence over the content of the website. The grumpy looking dentist with the outdated website could be the best oral surgeon in town, but chances are you passed him up because his website didn’t give you the impression of value, trust, or reliability. Instead you will remember the clean powder blue website with the round yellow logo in the corner – and in your opinion whoever this website belongs to, is the front runner in your search for a dentist. That’s your subconscious deciding.
Give People What They Want
As one of the founding partners of MyChiroPractice™, we have made it a mission to research and pinpoint what quality new patients look for when choosing a chiropractor, then designing a memorable brand and engaging online presence that resonates with them.
In a recent 100 person focus group study we conducted, 84% of participants said that TRUST supersedes experience and price when choosing a chiropractor online. So how can you portray trust through a website that looks cookie-cutter, outdated, and overwhelming with useless information? You can’t.
In other words, if you want to continue running a successful practice and attract quality patients, you have to come to grips with one simple (and difficult) concept; it doesn’t matter what you think looks nice, it’s important what your potential patients find attractive and engaging.
Three Things You Can Do Today to Evaluate Your Image
The first step in evaluating your website is to see if it is patient friendly. Take a look at your home page and see if it follows the 30/70 rule – whereas there is 30% text to 70% imagery. Why is this important? Besides the mere fact that consumers today don’t have the time or patience to read text-heavy content on a website, larger imagery can have much more of a psychological impact than its textual counterpart. By consolidating your paragraphs into a few short blurbs, you are opening the page to large rotating photos / banners, and presenting the patient all the relevant information they need on the home page, without a need to scroll.
The second step in evaluating your website is to ask yourself “does my website stand out from the competition?” To answer this question you must be 100% open to looking at it from a non-bias perspective. If your website looks eerily similar to most other chiropractic website out there – for the exception of some color changes or your logo – chances are potential quality new patients have picked up on that too, and will make certain assumptions about the quality of your practice.
Finally, does your website look cluttered, with an overwhelming number of tabs / buttons? Research shows that custom-designed websites with smaller page counts and intuitive navigation not only attract the attention of quality new patients, but portray a much higher value and quality of care. As a matter of fact, a recent focus group study conducted by MyChiroPractice™ revealed that 77% of potential patients leave a “cluttered” website within 2.2 seconds of arriving there.
SUMMARY
Whether we like it or not, the world is moving at a very fast pace. The sooner your chiropractic practice engages and attracts the new generation of patients, the sooner you can serve your community.
 Tuesday, July 17, 2012 at 11:08PM
Tuesday, July 17, 2012 at 11:08PM 
Private Practice Huntington Beach, CA
President Circular Traction Supply
CBP Instructor
INTRODUCTION
For years I have performed computerized range of motion testing on all of my new patients and again at periodic re-evaluations. I mostly did this testing to establish severity and document post-treatment improvement for me, the patient, and the insurance company. Since reading a book by Gray Cook, MSPT, OCS, CSCS entitled “Movement – Functional Movement Systems”, I now actual look at (and document) my patients ROM in both the up-right standing posture and the non-weight bearing supine position. Doing this helps me answer the following treatment questions:
I will demonstrate this type of flexibility analysis using the “Cervical Extension Test”, but please realize that this testing can be performed on the thoracic and lumbar spine as well as the extremities.
Cervical Extension Flexibility Test
Standing Test - The patient starts by standing erect with feet together, toes pointing forward. The patient then looks-up and tries to extend the head/face parallel with the ceiling. See Picture 1.
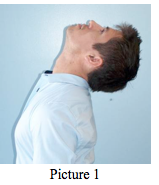
Picture 1
Supine Test – The patient assumes the supine position on a bench with the head and upper thoracic spine extending beyond the end of the bench. Have the patient try to extend their head/face perpendicular to the ground. See Picture 2.

Picture 2
By performing the flexibility test in this matter, the doctor is able to see if their patient’s restricted motion is being caused by their standing posture and their degree of flexibility in weight bearing vs. non-weight bearing positions.
1) If the patient has a notable forward head translation (more than 20 millimeters) and the:
Proposed dysfunction: The patient has a postural problem with associated motor control dysfunction. Look to your patient’s thoracic or lumbar/pelvic regions for the possible cause of the postural problem.
2) If the patient has a notable forward head translation and the:
Proposed dysfunction: The patient has a cervical/upper thoracic extension joint mobility/tissue extensibility dysfunction. This patient needs some form of cervical extension traction, supine axial extension traction or head retraction, depending on their neck/upper thoracic structure. Also, the prescription of head retraction exercises and an extension-based exercise device such as The Pro-Lordotic Neck Exerciser™ is indicated.
3) If the patient has a notable forward head translation and the:
Proposed dysfunction: The patient has a stability and motor control dysfunction. This patient needs a neuro-muscular treatment such as head-weighting performed walking or on a vibration platform or wobble device. See Picture 3.

DISCUSSION
“Mobility must precede stability” (1). This is a basic tenet of physical rehabilitation. The most obvious example of this tenet is a patient with a motion restricted ankle dysfunction. If you try to perform one-legged balance testing on this patient, they will not perform well. Not because of a deficiency of their ability to balance, but because of the deficiency of ankle ROM.
Altered posture alignment of any joint-structure can negatively affect mobility. This has also been found to be true. The most obvious example being that a person with a notable forward head posture will not have as much cervical ROM as a person with normal sagittal head posture.
SUMMARY
According to the above presentation, an effective rehabilitative treatment must first be aimed at improving posture and mobility before good neuromuscular stability can be expected.
These basic cervical flexibility tests presented above are intended as an aid to help the clinician determine the best postural corrective treatment for a patient. Please remember to always correlate your flexibility results with the patients structural x-ray findings and global posture to ultimately decide on their appropriate treatment.
Future articles will present selected case studies where this information is applied in the CBP Technique management of unique patient disorders.
Reference:
 Chiropractic BioPhysics
Chiropractic BioPhysics  Tuesday, July 17, 2012 at 11:07PM
Tuesday, July 17, 2012 at 11:07PM 
Randall Hammett, DC
Private Practice of Chiropractic
INTRODUCTION
After 33 years of practice and consulting with chiropractors around the country for approximately 20 years of this time, stress in everyday practice is normal. In fact, you need to depend upon having a stressful practice to a certain extent to be successful. I’ve seen through the years were chiropractic consultants purport the “stress less practice”. It’s been my observation that there is no such thing. The key is to balance the stress of everyday practice so that you can produce under stressful conditions and not be deterred by stress. There are basically two types of stress, the stress of loss and stress of gain. When your practice is doing well and growing exponentially you’ll find that there’s a certain type of stress involved in keeping the momentum and organization going. Conversely, when you practice is doing poorly there’s the stress of not being able to pay your bills or not living up to your expectations. Both of these stresses take their toll on your physical and mental well-being, so learning how to keep the stress in balance is paramount.
DISCUSSION
So, how do we handle the stresses from practice life? Although, I don’t have all the answers, Thirty three years in practice has rendered me some clarity on the subject. First and foremost, take care of your patient’s regardless of what’s going on in your personal or recreational life, inside the walls of your practice your patients are all and everything as well as your staff. As Dr. Gonstead said years ago, you only have one patient and that is the patient that is before you at the time you’re making your adjustment. Giving each patient total PTC allows you total freedom to go to the next patient knowing that you did the very best that you could each office visit. The key to balancing stress on a day-to-day basis is actually a simple formula that most fail to do, but is critical to living a simpler and more productive life.
First, have written goals, no more than five goals at a time is necessary. As you achieve each goal cross it off and add another. Each morning you should look at each of your goals and determine what’s necessary to achieve them. When you have a stressful event the goal should be near you to re-affirm what your plan and focus should be on. (We get what we focus on.) Without written goals you cannot achieve a balanced practice and personal life. It would also be a good idea for your staff and your family members to have goals also. Keep in mind that the goal should be short-term as in reachable within 12 to 18 months.
The next thing you need to do to minimize your stress is to get organized. Twice a year I go through my home and office and give away and/or donate any items I have not used in the prior year. I have found that the more items I have in my life the more the items begin to own me, instead of you owning them. Schedule time every six months for a cleanup and disposal day for yourself. Go through every drawer in your home and office and cleanup and throw out things you have not used in the last year. The next thing you need is a good calendar to remind you of events and to make plans. If you don’t have a smart phone I highly recommend that you get one with a good calendar. Everything should go on this calendar to help you get organized and get the excess crap out of your mind.
The third tool is to measure your progress towards your goals and this can be done by utilizing statistical analysis. Anything can be analyzed by numbers. It is important for you to be able to see the progress you are making from day-to- day and month to month basis. It is true that record keepers are record breakers and it amazes me how many chiropractors never keep statistical analysis of how well the practice is doing until tax time, which is a critical mistake.
SUMMARY
The last item is to not take anything too seriously. No one gets out of life alive and yes even chiropractors pass on to the great adjusting table in the sky. The goals you write should be both emotional and material with the idea that life is a very short ride and you should not waste time on things that aren’t directly under your control. The last thought you should keep in mind is this, that we are here on this planet to serve others and service to others is the ultimate life well spent.
Til next time,
 Tuesday, July 17, 2012 at 10:55PM
Tuesday, July 17, 2012 at 10:55PM 
Joe Betz, B.S., D.C
ICA Board Member,
PCCRP Board Member
Private Practice Boise, ID
Idaho Chiropractic Association Board Member
CBP Instructor
&
Jason Jaeger, DC
ICA Assembly Representative for NV
Nevada Chiropractic Association Board Member
CBP Instructor
Private Practice Las Vegas, NV
INTRODUCTION
Few things in daily practice are more time consuming and seemingly non-productive than time spent on documenting daily visits of patients. Perhaps the most concerning aspect of documentation pertains to the regulations on how to document appropriately for the Medicare daily visit. Doctors are being audited at alarmingly high rates. Audits from the Office of the Inspector General can result in the Chiropractor owing >$300, 000…all due to poor records. This isn’t exactly what one would consider malicious fraud, but it can result in serious repercussions.
Subluxation Documentation
The good news is that Medicare has defined what elements a clinical record from a chiropractor must contain for both the “Initial” and “Subsequent” encounters.1 It should first be stated that covered benefits for chiropractic are “only for treatment by means of manual and instrument manipulation of the spine to correct a subluxation.”1 Of note is the fact that Medicare requires the term, “Subluxation” be used in the treating chiropractor’s documentation. Exclusive use of other terms such “fixation” is not adequate.
A subluxation may be demonstrated by an X-ray and/or by physical examination. Although there are exceptions, the X-ray should have been taken at most 12 months prior to or 3 months following the initiation of a course of chiropractic treatment. Demonstrating the presence of a subluxation by physical examination is described in detail. The “PART” format is the acronym to remember the essential elements of the physical exam to demonstrate a subluxation: “Pain/tenderness evaluated in terms of location, quality, and intensity; Asymmetry/misalignment identified on a sectional or segmental level; Range of motion abnormality (changes in active, passive, and accessory joint movements resulting in an increase or a decrease of sectional or segmental mobility);and Tissue, tone changes in the characteristics of contiguous, or associated soft tissues, skin, fascia, muscle, and ligament.” 1
The manual continues, “To demonstrate a subluxation based on physical examination, two of the four criteria mentioned under “physical examination” are required, one of which must be asymmetry/misalignment or range of motion abnormality.”1 The history recorded in the patient record should include the following:
“Symptoms causing patient to seek treatment; Family history if relevant; Past health history (general health, prior illness, injuries, or hospitalizations; medications; surgical history); Mechanism of trauma; Quality and character of symptoms/problem; Onset, duration, intensity, frequency, location and radiation of symptoms; Aggravating or relieving factors; and Prior interventions, treatments, medications, secondary complaints.”1
Subluxation Documentation Requirements
“The following documentation requirements apply whether the subluxation is demonstrated by x-ray or by physical examination [Emphasis Added]:
DISCUSSION
It is important to note that individual states may have additional regulations described by their Medicare Administrative Contractor (MAC) in the form of a Local Coverage Determination (LCD).
The language used in the Medicare Benefit Policy Manual is precise in what is required. If you are not following Medicare’s described documentation requirements for the Initial visit on each and every Medicare patient, you are vulnerable to poor performance “when” (not “if”) they audit your records. You must own this information or suffer the consequences.
Electronic Health Record (EHR) systems that are properly designed will aid the chiropractor in documenting the Initial visit for a Medicare visit appropriately. This is perhaps the single most important aspect of choosing the proper EHR. Who are the clinical advisors? Do they understand the reality of Medicare documentation requirements? Be sure you can produce compliant notes, quickly and with confidence.
A system such as this would simplify the doctor’s life, the staff requirements. A system like this would set the clinic using it, above and apart from the rest.
SUMMARY
To realize this unprecedented professional standard now required by Medicare, CBP has partnered with a well known-respected EHR Company to develop a system specifically for CBP and corrective care doctors. This system will debut at the 2012 CBP Annual conference in Scottsdale, AZ at the Boulders Resort. See the annual conference ad in this issue or go to www.idealspine.com for registration.
References
1. Medicare Benefit Policy Manual. Chapter 15 Section 240. Chiropractic Services.
 Chiropractic,
Chiropractic,  documentation,
documentation,  medicare,
medicare,  subluxation
subluxation  Tuesday, July 17, 2012 at 10:53PM
Tuesday, July 17, 2012 at 10:53PM Practice Coach and Mentor
INTRODUCTION
I receive calls from doctors all over the country asking me one of the most common questions, “How do I have MORE patients stay for a lifetime?” My answer? “5 Steps.”
In Elite Coaching, we have a strong core value that patients should have an optimal spinal structure to attain optimal health. Isn’t that the principle of Chiropractic? We also believe each patient and family members should live their WHOLE LIFE with an optimal spine for optimal health. How do we take a patient saying, “Doc, fix my back,” to “I want to change the way I live my life for me and my family?” This is a system and this system works. Just ask the docs using it.
First of all, if you want to change the way people act you have to change the way they think. Unfortunately, you are not going to change the way they act and think until you find out how they FEEL, NOT what they THINK. You see, Subluxation is a fact. Facts are processed in the Cerebral cortex. The cortex processes facts, language and rational thinking. There is no decision making in the cortex.
The Limbic brain processes emotion and assigns an emotion to every experience. It does not rationalize, process facts and is TOTALLY responsible for behavior. Hence, the adage, “People buy with emotions and justify with fact.” Even a person who buys from facts and information TRUSTS information. Trust is processed in the Limbic brain. Therefore, if you are going to inspire people you MUST speak to their Limbic brain. This requires a different language, the language of emotion.
In a Consultation we address their pain and we focus on their organs. This is through system of communication discovering how they FEEL about their organ problems. EVERY person has a feeling about their health problems. When you discover they have high blood pressure and are scared of a heart attack, hypoglycemia and fear diabetes, fatigued and frustrated, and have them SAY, “I don’t want to be like this anymore,” on Day #1, you have taken a HUGE first step into their emotion. Before they know what they want, they must know what they DON’T want.
The late Dr. Don Harrison and his son, Dr. Deed Harrison teach an overwhelming amount of research in CBP seminars proving subluxated postures lead to disease and early death. How do your patients learn this? Dr. Deed and Elite Coaching have come together to create the, “Regaining Your Youth & Vitality,” new patient workshop with a number of these studies. It handles almost every patient objection and is VERY obvious to every patient in the room their posture is affecting every area of their life, including life span. This workshop creates an emotional response (Limbic Brain).
To me, the worst insult is finding myself trying to convince a patient into accepting care for their own good. NO MORE! Have them tell you what THEY want. When they write their 20-30 year life goals they are telling you how to speak to their emotion (Limbic Brain) by knowing their highest priority. Now get them 100% committed to that life and have the patient say they can’t live that life if they allow their subluxated posture to progress. NOW they are buying the life they want rather than your program (Limbic Brain). Then give them the recommendations, the solution to their BIGGEST problem. FYI, “Entrepreneurs solve people’s problems for a profit.” T. Harv Eker “Secrets of a Millionaire Mind.”
Your re-exam reminds them of their original organ problems, their original level of health, shows improvement and sets short term goals on the healing of their organ problems. People forget where they came from and become unappreciative and lose the emotion. They adapt to their new state of health. Remind them and bring out their 30 year goals every 30 days to keep their attention on their vision (Limbic Brain). Next, ask them to repeat their whole corrective and maintenance program into lifetime care every 30 days. Make the transition into lifetime care seamless with your financials.
Have a club they enter when they have completed postural correction. Make a BIG DEAL about it. Stencil it on a wall with their picture to give them a visual goal (Limbic Brain). Take their picture in the middle of the adjusting area at your busiest time. Present them with a membership plaque in front of other patients and watch how many patients will inquire and make that their goal (Limbic Brain). Set a goal for how many patients enter the club and watch your practice go through the ROOF!
SUMMARY
We are teaching these principles of how to create lifetime patients and MUCH more at our Elite Coaching Las Vegas seminar, August 25th/26th, 2012. Dr. Deed Harrison is one of our phenomenal speakers. Please call us today to attend at 253-851-5899, or call me, Dr. Fred DiDomenico, personally at 253-851-8353 for any questions.
 CBP,
CBP,  Chiropractic BioPhysics,
Chiropractic BioPhysics,  Elite Coaching
Elite Coaching  Tuesday, July 17, 2012 at 10:48PM
Tuesday, July 17, 2012 at 10:48PM Co-Owner Developer of the Chiropractic Business Academy
drhuntington@chirobizacademy.com
INTRODUCTION
Yes, I’m talking about that feeling most get once in practice about ten years. It comes earlier for some, and maybe later for others. But I think we all get it. More about that in a moment.
I think that we are all very fortunate to have chosen chiropractic—or, as some suggest, maybe chiropractic chose you. Either way, if you’ve been in practice for ten or more years, I hope you have enjoyed being a chiropractor as much or more than I have enjoyed it.
At the same time, being in this profession comes with some challenges. Hopefully you knew that when you signed up for this game. For an easier time you could have become a stock broker, an attorney, or even a medical doctor. Maybe those professionals would argue with me on this point, but I’m pretty sure that the chiropractor has a tougher, but in my opinion, more rewarding path.
For most, this is a rather disturbing thought. Some probably push it away, out of site, rather than think about it. Unfortunately, doing so does not solve the problem, and actually shortens the amount of time you have to handle it!
The simple fact is, not all of us are blessed with a body that will allow us to continue practicing past a certain point. And for others, it’s not the physical barrier, but a mental one.
Although things like chiropractic research, or philosophy can be mentally stimulating, the day to day practice of chiropractic for the doctor in practice is rather mundane. The fact is, treating patients is very repetitive and very physical and is only interrupted occasionally by brief moments requiring relatively complex analytical decisions. It’s just the nature of the typical chiropractic practice and is more a comment on most jobs than on the profession itself.
Now, combine those facts with being a health care provider outside the mainstream medical and insurance systems. To make matters more difficult, most chiropractors have few business skills, and yet own and operate a private practice. This typically results in many years of “figuring it out” with only a few years of good success and income.
It all adds up to, “I love what I do, and it’s been good to this point, and I’d love to continue doing something in chiropractic in some way, but I’ve got to earn more income or else I will never retire, and my body is going to demand that I ‘retire’ at some point not to mention, I’d like a real vacation one of these days”.
DISCUSSION
So… What options does a chiropractor have at this point?
This is probably the most commonly chosen option. Possibly due to some degree of non-confront on the part of the doctor, “this isn’t really happening” or “I won’t let this happen” and/or because the doctor does not know what else to do-- it’s easier to do what you know rather than to figure out a new solution. Unfortunately, this strategy does not win in the long run and wastes valuable time that could be used to create a real viable future.
This option is pretty apathetic and is indicative of not knowing what else to do. It’s a slow death for the practice, as well as the career and finances of the doctor. Few can afford to do this.
This is only slightly better than the second option. It’s a slow death with a bit of financial first aid.
Now here is a good idea! However, we should be more specific about how to do this because there is probably an infinite number of ways to do this wrong and a limited number of ways to do this right. The key is, hiring staff, including an associate, and growing the practice. This is the most viable long-term option. It helps new grads too!
Many hundreds of CBA clients all over the country are either on their way to building, or have already created very profitable, staff-run practices. These doctors earn more income and often work less than they ever have in the past.
The ability to do this is not natural to most people. The good news is that it is completely within the ability of most chiropractors to learn!
SUMMARY
If you would like to learn about the CBA approach to building a highly profitable practice that runs with or without you, call CBA today and speak to one of our consultants.
Call Now 888-989-0855
Tell the consultant that you want to learn the CBA system that gets staff to do the work! Our consultant will show you the exact system we teach our clients. If you are bright, and really participate in learning from this free consultation, you may be able to improve your practice even without any further help from CBA.
From the French Polynesian island of Moorea, I am postulating for you the future of your dreams!
 Tuesday, July 17, 2012 at 10:43PM
Tuesday, July 17, 2012 at 10:43PM
CBP Research & Instructor
Private Practice New Market, Ontario, Canada
ABSTRACT
Objective: To investigate the effects of lumbar extension traction in patients with unilateral lumbosacral radiculopathy due to L5–S1 disc herniation.
Design: A randomized controlled study with six-month follow-up.
Setting: University research laboratory.
Subjects: Sixty-four patients with confirmed unilateral lumbosacral radiculopathy due to L5–S1 disc herniation and a lumbar lordotic angle less than 39°, randomly assigned to traction or control group.
Interventions: The control group (n = 32) received hot packs and interferential therapy, whereas the traction group (n = 32) received lumbar extension traction in addition to hot packs and interferential therapy.
Main outcome measures: Absolute rotatory angle, back and leg pain rating scale, Oswestry Disability Index, Modified Schober test, H-reflex (latency and amplitude) and intervertebral movements were measured for all patients three times (before treatment, after 10 weeks of treatment and at six-month follow-up).
Results: There was a significant difference between the traction group and the control group adjusted to baseline values at 10 weeks post treatment with respect to: absolute rotatory angle (P < 0.001), Oswestry Disability Index (P = 0.002), back and leg pain (P = 0.009, P = 0.005), Modified Schober test (P = 0.002), latency and amplitude of H-reflex (P = 0.01, P < 0.001), intervertebral movements (P < 0.05). At six-month follow-up there were statistically significant differences between the study and control groups for all the previous variables (P < 0.05).
Conclusion: The traction group receiving lumbar extension traction in addition to hot packs and interferential therapy had better effects than the control group with regard to pain, disability, H-reflex parameters and segmental intervertebral movements.
ABSTRACT
Objective: The purpose of this study was to investigate the effects of lumbar extension traction with stretching and infrared radiation compared with stretching and infrared radiation alone on the lumbar curve, pain, and intervertebral movements of patients with chronic mechanical low back pain (CMLBP).
Methods: This randomized clinical study with 3-month follow-up was completed at the Cairo University research laboratory. Eighty patients (age ranged from 40 to 50 years) with CMLBP and a hypolordotic lumbar spine were randomly assigned to traction or a comparison group. The comparison group (n = 40) received stretching exercises and infrared radiation, whereas the traction group (n = 40) received lumbar extension traction in addition to stretching exercises and infrared radiation. The absolute rotatory angle, intervertebral movements, and visual analog scale were measured for all patients at 3 intervals.
Results: The results revealed a statistically significant difference between the groups at 2 follow-up time points compared with the baseline values for the translational and sagittal rotational movements of L3-L4, L4-L5, L5-S1, and L2-L3(post treatment) and absolute rotatory angle (P < .01). There were no statistically significant changes in pain (P = .1 and .3) and L1-L2 (P = .072 and .076) or L2-L3 (at follow-up; P = .3), and there was no significant difference between all the previous variables adjusted to the groups' baseline outcome interaction (P > .01).
Conclusion: Lumbar extension traction with stretching exercises and infrared radiation was superior to stretching exercises and infrared radiation alone for improving the sagittal lumbar curve, pain, and intervertebral movement in CMLBP.
 Tuesday, July 17, 2012 at 10:31PM
Tuesday, July 17, 2012 at 10:31PM CEO and Founder of Neuromechanical Innovations
A ISO 13485 Certified Medical Device manufacturer of the Impulse® family of adjusting instruments, based in Chandler, Arizona.
Prominent Spine Researcher and Reviewer
He can be reached at DrC100@aol.com or at www.neuromechanical.com
INTRODUCTION
Inherent in the definition of chiropractic adjustment is the need to identify abnormal mobility and/or alignment and the introduction of specifically applied forces intended to reduce or correct the dysfunction. Inasmuch, over a decade ago, I placed my research focus into developing technology geared towards the ability to quantify spinal displacements and monitor spinal motion responses during chiropractic adjustments. With this agenda, I assembled an international research team to examine the biomechanical characteristics of various spinal pathologies and their relationship to spinal motion. Born out of this research was a validated non-invasive spinal stiffness assessment methodology that compared our methods to a gold-standard intersegmental motion technique that we published in 2009 in the journal, Spine (Colloca et al. 2009). Forces that are relatively large in magnitude, but act for a very short time (much less than the natural period of oscillation), are called impulsive.
Quantifying Spinal Pathology
Segmental instability and pathology of the spine are believed to produce abnormal patterns of motion and forces, which may play a significant role in the etiology of musculoskeletal disorders (Nachemson 1985). The ability to quantify in vivo spine segment motion (displacement) and stiffness (force/deformation) in response to forces is thus considered to be of clinical significance in terms of both diagnosis and treatment of spinal disorders. Moreover, knowledge of spine segment motion patterns, forces and stiffness is also of fundamental interest to understanding the postural, time-dependent and dynamic response of the spine, the role of spinal implants in mechanical load sharing, and the response of the extremities (appendicular skeleton) and spine (axial skeleton) to externally applied forces such as chiropractic adjustments (Keller et al. 2002).
The mechanical and physiologic response of the spine to PA forces is dependent upon many factors, including the intensity, direction, duration and frequency of the applied force. Of these factors, the frequency-response and frequency-dependent stiffness characteristics of the spine to PA dynamic loading is perhaps the least well understood. The dynamic PA frequency-dependent stiffness behavior of the human spine reflects the fact that the spine is a viscoelastic structure, albeit generally more elastic than viscous. Different structures (ligaments, cartilage, bone, tendons, muscle) will exhibit varying degrees of time-dependent and frequency-dependent viscoelastic behavior. Consequently, the overall structural/vibration response of the spine is modulated by both the architecture or structural organization of component tissues as well as load sharing provided by adjacent structures (e.g. rib cage, sternum, pelvis). When such factors are combined with other considerations such as spinal curvature, the net effect is a complex structure-frequency-dependent mechanical behavior.
The general approach for determining the dynamic response of a man-made or biologic structure consists of simultaneously measuring an excitation or input signal (typically force) and response or output signal (displacement, velocity or acceleration) in the time domain and analyzing them in the frequency domain. Two principal types of frequency response transfer functions can be determined: a ratio of like parameters such as the ratio of the force transmitted to the disturbing force (transmissibility), or a ratio of two dissimilar parameters such as the ratio of the disturbing force to the velocity transmitted (mechanical impedance). Frequency response functions, together with identification of the resonant frequencies associated with the vibration, provide important information concerning the mechanical behavior of the structure. For example, when the spine is dynamically loaded along the PA direction a lower impedance value implies that the intervertebral joints are easier to excite and capable of greater mobility and storage of larger amounts of energy, whereas the opposite holds for transmissibility (Kazarian 1972). A variety of mechanical vibration “transfer functions” can be defined for various excitation (input) and response (output) signals (Table 1).
Table 1. Dynamic Frequency Response Transfer Functions
Name |
Transfer Function |
|
Accelerance |
acceleration/force (kg-1) |
|
Effective Mass |
force/acceleration (kg) |
|
Mobility |
velocity/force (m/Ns) |
|
Impedance |
force/velocity (Ns/m) |
|
Compliance |
deformation/force (m/N) |
|
Stiffness |
force/deformation (N/m) |
A very fast and efficient method to determine the broadband dynamic mechanical response of a structure is to use transient testing techniques such as impact testing. During impact testing, a hand-held instrument (typically a hammer) with a load cell mounted to it is used to deliver a force impulse to the structure, and the motion response is measured using an accelerometer either mounted to the structure or mounted directly to the instrument (driving-point). It is this technique that we have refined and patented for our unique approach of simultaneously monitoring spinal motions during chiropractic adjustments. In the next issue of the Journal, we will review the benefits of adjusting at the resonant frequency of the spine.
References
 Neuromechanical Innovations
Neuromechanical Innovations 