Flexibility Testing and its Implications to Corrective Care
 Tuesday, July 17, 2012 at 11:08PM
Tuesday, July 17, 2012 at 11:08PM 
Private Practice Huntington Beach, CA
President Circular Traction Supply
CBP Instructor
INTRODUCTION
For years I have performed computerized range of motion testing on all of my new patients and again at periodic re-evaluations. I mostly did this testing to establish severity and document post-treatment improvement for me, the patient, and the insurance company. Since reading a book by Gray Cook, MSPT, OCS, CSCS entitled “Movement – Functional Movement Systems”, I now actual look at (and document) my patients ROM in both the up-right standing posture and the non-weight bearing supine position. Doing this helps me answer the following treatment questions:
- When does the aberrant posture require strong traction?
- When does the aberrant posture require more of a neuromuscular treatment?
- When is the aberrant posture the primary problem and not just a compensation of some other problem?
I will demonstrate this type of flexibility analysis using the “Cervical Extension Test”, but please realize that this testing can be performed on the thoracic and lumbar spine as well as the extremities.
Cervical Extension Flexibility Test
Standing Test - The patient starts by standing erect with feet together, toes pointing forward. The patient then looks-up and tries to extend the head/face parallel with the ceiling. See Picture 1.
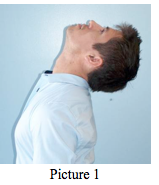
Picture 1
Supine Test – The patient assumes the supine position on a bench with the head and upper thoracic spine extending beyond the end of the bench. Have the patient try to extend their head/face perpendicular to the ground. See Picture 2.

Picture 2
By performing the flexibility test in this matter, the doctor is able to see if their patient’s restricted motion is being caused by their standing posture and their degree of flexibility in weight bearing vs. non-weight bearing positions.
- Theoretical Observations from these tests:
1) If the patient has a notable forward head translation (more than 20 millimeters) and the:
- · standing extension is poor,
- ·
Proposed dysfunction: The patient has a postural problem with associated motor control dysfunction. Look to your patient’s thoracic or lumbar/pelvic regions for the possible cause of the postural problem.
2) If the patient has a notable forward head translation and the:
- · standing extension is poor,
- ·
Proposed dysfunction: The patient has a cervical/upper thoracic extension joint mobility/tissue extensibility dysfunction. This patient needs some form of cervical extension traction, supine axial extension traction or head retraction, depending on their neck/upper thoracic structure. Also, the prescription of head retraction exercises and an extension-based exercise device such as The Pro-Lordotic Neck Exerciser™ is indicated.
3) If the patient has a notable forward head translation and the:
- · standing extension is good,
- · supine extension is good .
Proposed dysfunction: The patient has a stability and motor control dysfunction. This patient needs a neuro-muscular treatment such as head-weighting performed walking or on a vibration platform or wobble device. See Picture 3.

DISCUSSION
“Mobility must precede stability” (1). This is a basic tenet of physical rehabilitation. The most obvious example of this tenet is a patient with a motion restricted ankle dysfunction. If you try to perform one-legged balance testing on this patient, they will not perform well. Not because of a deficiency of their ability to balance, but because of the deficiency of ankle ROM.
Altered posture alignment of any joint-structure can negatively affect mobility. This has also been found to be true. The most obvious example being that a person with a notable forward head posture will not have as much cervical ROM as a person with normal sagittal head posture.
SUMMARY
According to the above presentation, an effective rehabilitative treatment must first be aimed at improving posture and mobility before good neuromuscular stability can be expected.
These basic cervical flexibility tests presented above are intended as an aid to help the clinician determine the best postural corrective treatment for a patient. Please remember to always correlate your flexibility results with the patients structural x-ray findings and global posture to ultimately decide on their appropriate treatment.
Future articles will present selected case studies where this information is applied in the CBP Technique management of unique patient disorders.
Reference:
 CBP Seminars | Comments Off |
CBP Seminars | Comments Off |  Chiropractic BioPhysics
Chiropractic BioPhysics