Paul Oakley, MD, DC
Paul Oakley, MD, DC
INTRODUCTION
Ergonomics is not adequately taught to the chiropractic student.1 It is not until in practice that the chiropractor experiences frustration for particular cases of patients who just don’t get better! Oftentimes, it is these patients who are compromising their chiropractic care by unknowingly and inadvertently partaking in movements and physical tasks that are overstressing the spine and posture resulting in a continuation of nociceptive tendencies. This is why ergonomics is so important in daily practice.
It is important to emphasize that ergonomics is not always easy or simply black and white in its application - “there is no magic answer.”2 That is, general biomechanical principles must be realized then applied appropriately to specific tasks accommodating any special needs of the patient. With this in mind it is good practice to get feedback from the patient when suggesting appropriate ergonomic recommendations so as not to overlook any critical factor, as most advice will be offered without performing a direct task analysis. In addition, this practice involves the patient in the solution process motivating their participation. Blind doctor recommendations for patient ergonomic issues is not optimal, therefore, educating the patient on general concepts so the solution can be cooperatively contrived between the doctor and patient is advised. Tough cases, however, may require ergonomic assessment by those with expertise.
The CBP® Doctor knows that the efficacy of common back treatments are poor.3 Even newer approaches involving evidence-based spine stabilization protocols (See McGill, 2002) admit to failure for so-called ‘failed’ backs. The reason for common LBP treatment failures are probably two fold. First, as eminently stated by McGill “those paying for injury could reasonably argue …that, to reduce costs, care for the injured back should be removed from medical hands and given to ergonomists.”4 No treatment will be effective if the contributing ergonomic factors are not eliminated or reduced. Second, only CBP traction procedures have been proven to restore the normal structure of the lumbar posture.5 In fact, only with a normal lumbar posture static posture will one have normal dynamic functioning, the simple concept of ‘Structure determines Function,’ a concept which has been established throughout the spine.6-8
- Five Key Concepts to Lumbar Spine Ergonomics:
- Maintain the Neutral Lumbar Lordosis
- Appropriate Timing of Spinal Loads
- Optimal Spinal Loading: Not too much, not too little
- Reduce the Reaction Moment
- Maintain Spine Stability
Part 1 of this series of articles will review the first two contemporary ergonomic concepts to aid the CBP doctor in helping their patients’ needs to eliminate ergonomic related obstacles for optimum structural rehabilitation of the lumbar spine.
- Maintain the Neutral Lumbar Curve
Many have stressed the importance of maintaining the normal lordotic curve during the performance of tasks such as lifting and sitting. This is important due to the fact that “maintaining a more neutrally lordotic spine will maximize shear support, ensure a high tolerance of the joint to withstand compressive forces, eliminate the risk of ligamentous damage since the ligaments remain unstrained, (and) eliminate the risk of disc herniation since this is associated with a fully flexed spine.”4
- Sitting:
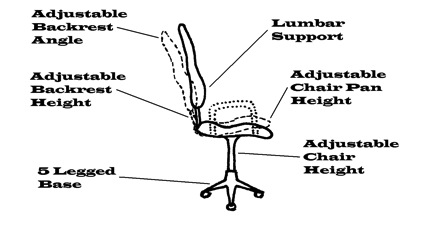
While seated a lumbar support should be used! Fortunately most seating now incorporates this aspect into its design. Since the low back is elliptical in configuration, it is of no surprise that lumbar support provided over the L4-5 area is preferred over higher locations.9 Caution should be taken to not position a support too low thereby translating the pelvis forward in the seat or too high which flattens the lumbar spine.10 The combination of tilting the seat backrest up to 120° in combination with a 5cm lumbar support has an optimal effect of reducing lumbar disc pressures.11 Arm rests also reduce up to 25% of low back loads12 by reducing disc pressures and myoelectric activity.13 A good computer chair should have at least four ‘degrees of freedom’ or adjustable features.14;15 See Figure 1.
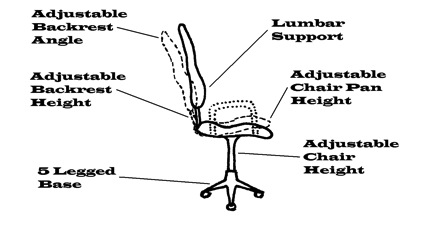 Figure 1: A good chair should have several adjustable features.
Figure 1: A good chair should have several adjustable features.
- Lifting:
When lifting the common adage of ‘lift with your legs, not your back’ is a myth! This has been propagated since the 1930s16;17 and has not reduced the incidence in low back injuries.18 In fact, many have questioned the validity of such a thing as a single universal lifting technique.17;19;20 This is because above all else the goal to lifting should be to: 1) Reduce the reaction moment (ie. by carrying objects close to the body) which reduces the extensor forces and the resultant compressive low back loading; 2) Avoid a fully flexed posture (ie. maintain the neutral lordosis by bending at the hips) which minimizes low back shear loading.21 One method to maintain the lordosis while picking up light objects is to perform the golfer’s lift. This involves bending the neutral torso over a single hip to reach down while balancing the body with the other leg out behind. It should now be apparent that by satisfying these two criteria that many postures may be successfully used to accomplish a safe lift.
- Appropriate Timing of Spinal Loads
When considering the order of activity performance, one must appreciate that the spine has a loading memory.21;22 That is, prior activity modulates subsequent spine function. The spine may be at significant risk of a destabilizing injury after either cyclic or sustained loading.23 This is due to the viscoelastic tissues of the spine. For example, after cyclic loading (ie. repeated lifting), laxity in the soft tissues causes a reduced protective muscular reflexive activity due to mechanoreceptor desensitization.23 Thus, a lifting activity should not be performed immediately following prolonged sitting or stooping and repetitive tasks. Instead the patient should recover spine stability (achieve redistribution of the nuclear material and recover ligament stiffness)24;25 by simply standing (which is a good rest from sitting),26 or consciously extend the spine (easily achieved by reaching for the ceiling).4 Walking for five minutes could also be recommended prior to lifting24 especially if preceded by prolonged vibration.27
The spine has a diurnal variation that affects its biomechanics and ultimately its injury mechanics. In fact, intervertebral disc-bending stresses are 300% and ligament stresses are 80% greater after rising from bed in the morning than later in the afternoon.28 This is why it may be a dangerous practice to perform early morning full range flexions of the spine as would be required of lifting and stooped postures. Snook et al. (1998)29 have demonstrated that simply avoiding full flexion early in the morning is a successful strategy for recovering LBP patients. After 30 minutes of upright posture, 54% of the daily disc height loss is achieved which reduces the potential risk of early morning back flexions, after 3 hours one loses about 80% of the total daily height loss!30
It is a wise recommendation to avoid full flexion postures soon after rising including those that may be a part of a daily exercise routine especially for those undergoing rehabilitation. This is one concept that is critically important. I have seen on many occasions where a patient starts to respond to care, then one day confesses frustration that they are not getting any better or regressing. Upon questioning them I invariable discover that they are so motivated to get well they never skip their intensive early morning stretches – of course, excessively flexing their backs first thing in the morning and therefore damaging their disks! Tell your patients to stretch later in the day, at least after lunchtime. Taking garbage out to the curb the night before garbage day is another good example of using this principle.
See the next issue of the AJCC for the continuation of the 5 key contemporary ergonomic concepts.
References---See AJCC Online for detailed list of references accompanying this article
10. Andersson GBJ, Murphy RW, Ortengren R, Nachemson AL. The influence of backrest inclination and lumbar support on lumbar lordosis. Spine 1979; 4(1):52-58.
11. Chaffin DB, Andersson GBJ. Occupational biomechanics. 2 ed. John Wiley & Sons, New York, 1991
12. Cailliet R. Neck and arm pain. 3 ed. F.A. Davis Company, Philadelphia, 1991
13. Andersson GBJ, Ortengren R. Lumbar disc pressure and myoelectric back muscle activity during sitting. III. Studies on a wheel chair. Scand J Rehab Med 1974; 6:122-127.
14. Scalet EA. VDT health and safety: Issues and solutions. Ergosyst Associates, Lawrence, Kansas, 1987
15. Carter JB, Banister EW. Musculoskeletal problems in VDT work: A review. Ergonomics 1994; 37(10):1623-1648.
16. U.S.Preventive Services Task Force. Screening for risk of low back injury. Guide to clinical preventive services: An assessment of the effectiveness of 169 interventions. Williams & Wilkins, Baltimore, 1989, pp. 245-249.
17. Parnianpour M, Bejjani FJ, Pavlidis L. Worker training: the fallacy of a single, correct lifting technique. Ergonomics 1987; 30(2):331-334.
18. Brown JR. Lifting as an Industrial Hazard. 1972. Labour Safety Council of Ontario, Ontario Department of Labour.
19. Graveling RA, Simpson GC, Sims MT. Lift with your legs, not with your back: a realistic directive? Brown ID, Goldsmith R, Coombes K, et al., editors. 910-912. 1985. London, Taylor & Francis. Ninth Congress of the International Ergonomics Association.
20. Chaffin DB, Park KS. A longitudinal study of low back pain as associated with occupational weight lifting factors. Am Ind Hygiene Assoc 1973; 34:513-525.
21. McGill S. The biomechanics of low back injury: Implications on current practice in industry and the clinic. Journal of Biomechanics 1997; 30(5):465-475.
22. McGill SM. Biomechanics of low back injury. 22-23. 1995. XV International Society of Biomechanics. July 2-6, Finland.
23. Solomonow M, Zhou BH, Baratta RV, Lu Y, Harris M. Biomechanics of increased exposure to lumbar injury caused by cyclic loading: Part I. Loss of reflexive muscular stabilization. Spine 1999; 24(23):2426-2434.
24. McGill SM, Brown S. Creep response of the lumbar spine to prolonged full flexion. Clinical Biomechanics 1992; 7:43-46.
25. Magnusson ML, Aleksiev AR, Spratt KF, Lakes RS, Pope MH. Hyperextension and spine height changes. Spine 1996; 21(22):2670-2675.
26. Callaghan JP, McGill SM. Low back joint loading and kinematics during standing and unsupported sitting. Ergonomics 2001; 44(3):280-294.
27. Pope MH, Magnusson M, Wilder DG. Low back pain and whole body vibration. In: Kumar S, ed. Biomechanics in ergonomics. Taylor & Francis, Philadelphia, PA, 1999, pp. 233-241.
28. Adams MA, Dolan P, Hutton WC. Diurnal variations in the stresses on the lumbar spine. Spine 1987; 12(2):130-137.
29. Snook SH, Webster BS, McGorry RW, Fogleman MT, McCann KB. The reduction of chronic nonspecific low back pain through the control of early morning lumbar flexion. Spine 1998; 23:2601-2607.
30. Reilly T, Tyrrell A, Troup JDG. Circadian variation in human stature. Chronobiology International 1984; 1(2):121-126.
 Tuesday, July 17, 2012 at 10:53PM
Tuesday, July 17, 2012 at 10:53PM  CBP Seminars | Comments Off |
CBP Seminars | Comments Off |  CBP,
CBP,  Chiropractic BioPhysics,
Chiropractic BioPhysics,  Elite Coaching
Elite Coaching